Cornea DALK DSEK DMEK DWEK or DSO
What is a Cornea?
The cornea is the outermost part of the eye. It is made up of many layers of thin cells. It is clear, therefore we are not able to see it. The first structure of the eye we perceive is the iris which is the colored area: brown, blue, or green are the normal colors.
The cornea is masterfully crafted by nature. Even the most expensive man-made lenses cannot match its accuracy of function and self-preservation. The smoothness and shape of the cornea is critically important to its proper functioning as well its transparency. If either the surface level of smoothness or the quality of the cornea is altered, vision will come to be compromised.
Although appearing to be one clear membrane, the cornea is really composed of five distinct layers of tissue, each with its own function. The slim outer layer, or epithelium, is a dependable obstacle against corneal infection. It normally has to be damaged before an infectious bacteria or virus can enter between the layers of the cornea. Just below this layer is a fibrous band called Bowman’s membrane. It is important for the integrity of the cornea.
The third layer called the stroma is constructed from collagen, a connective tissue. This forms eighty percent of the cornea. Besides collagen fibrils, there are cells called keratocytes. The density of the fibres is higher towards the Bowman’s membrane. Below the stroma is again a fibrous layer. This is termed as Descemet’s membrane. It is the scaffolding for the innermost layer of cells called Endothelium cells.
When endothelial cells are healthy and balanced, they function as a “pump-leak system” to provide nutrients for the cornea. In other words these cells allow nourishing fluid from inside the eye (liquid food) to leak into the cornea. After the corneal cells have actually been nourished, the cells pump the fluid from the cornea.
If the endothelial pump is compromised for any reason the cornea will certainly over hydrate as well as become hazy. This most frequently takes place in patients that have suffered injury to the endothelial layer during complex cataract surgical procedure or individuals that have actually acquired an illness of the corneal endothelium referred to as Fuchs’ Endothelial Dystrophy.
A corneal transplant works like replacing the windshield of a car. When we drive during different times of the day we need to be able to see through the windshield out into the distance. The windshield needs to be clear at all times. Dust or rain can impair our ability to see through it. Likewise the cornea has to be always kept clear.
Light travels through the clear cornea on its course toward the retina in the back component of the eye. A healthy, clear cornea is needed for perfectly clear vision. Sometimes, the cornea is referred to as the” window” to the eye. Occasionally, either through disease or injury, the corneal tissue is harmed to a point where light could no longer successfully pass through it, causing reduced vision.
Cornea Transplant or Corneal Transplantation?
Cornea transplant is the removal of the diseased cornea of a patient and replacing it with a new cornea from a generous deceased person.
There are a wide number of individuals that suffer from a diseased or cloudy cornea. When this particular area of the eye begins to have trouble, light cannot pass through this area successfully which results in blurry vision or even blindness. When this happens, it’s up to your ophthalomologist or an eye doctor to decide the best treatment for your specific condition. Now, it’s important to understand that simply because the cornea is having a problem, before a corneal transplant can take place, it will have to be determined that the retina as well as nerve at the back of the eye is completely healthy.
Indications for Cornea Transplant
Any dense scarring or opacity in the cornea. This affects the vision and cannot be improved with glasses or contact lenses. We can classify the causes:
- Congenital – Opacity like Peters anamoly
- Degenerative – Keratoconus, Macular cornea degeneration, Fuchs dystrophy
- Trauma – Like central corneal injury
- Tumors – Keloid
- Pterygium which invades central cornea
- Post surgical – Pseudophakic Bullous Keratopathy.
Once this has been determined, your doctor can decide whether or not this is the correct technique that will need to take place. Now, corneal transplantation is exactly what it sounds like. Your cornea is being transplanted with a new donated cornea. If you have been diagnosed successfully, and it has been decided that a transplant technique will work in your specific case, this is an option you will have – provided the new donated cornea is available.
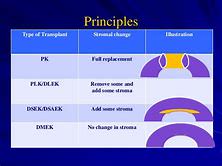
Types of Cornea Transplant
- Full thickness Cornea graft called Penetrating Keratoplasty or PK
- Lamellar Graft or LK
- DALK or Deep Anterior Lamellar Graft
- DSEK or Descemets Stripping Endothelial Keratoplasty
- DMEK or Descemet Membrane Endothelial Keratoplasty
- DWEK OR DSO – Descemets membrane stripping
Traditionally manual keratomes have been used. We have now started using femtosecond lasers to get better shape alignments.. This helps in increasing wound apposition, strength and at the same time decreasing induced astigmatism.
The exact type of cornea transplant best suited for you can be determined by a cornea surgeon like Rajesh Khanna, MD based in Los Angeles area. Call him at (310) 482 1240 if you need to find what is BEST for you.
Why Choose a Cornea Transplant ?
There are many individuals that will wonder why they should choose a corneal transplant other than any other technique available. Well, this is a question that can only be answered with regards to your specific situation. It’s important to understand that everyone is different, and everyone will suffer with a different eye condition. Each condition will not require this type of technique. However, you’ll be happy to know that if you have been diagnosed thoroughly, and they find that this is a technique that can be used in your specific situation, you can benefit a great deal by having this procedure performed.
* The Benefits of Corneal Transplantation
One of the major benefits of corneal transplantation will be the fact that you can see again. Now, it’s important to note that you will have to undergo some healing time, but if all of the diagnostic procedures have been performed extensively, you’ll discover that this is a procedure that takes very little time and as a result of completion you will be able to see again. It’s important to note that with any type of procedure available, there can be complications; however, 99.9% of the people that have been diagnosed for this technique have successfully regained their eyesight to a positive degree.
So, when it comes to corneal transplantation, this is another option that is available for those that have been having corneal issues that are unresolved. As stated before, it will be important for you to work with your optometrist or eye doctor to determine whether or not this is a technique that will provide you with great benefits.
Cornea transplant and Insurance Coverage
There are certain costs involved in cornea transplant procedure. They can be divided into
- Cost of the cornea from the eye bank
- Cost of the surgery center
- Surgeon fees
- Anesthetist fees
- Laser fees
- Preoperative measurements
- Follow up care
Usually medical insurance covers some or most of the cost. Vision Insurance does not apply to this procedure. She insurances have stopped covering costs for the Cornea graft. It is best to send us your medical insurance card in advance so we can check your coverage.
Preparing for the Cornea Transplant procedure
A lot of arrangements are made by the surgeon, eye bank and the surgery center to procure the cornea and have it ready for cornea transplant surgery. It is imperative you do not try to reschedule the surgery unless its absolutely medically necessary.
On the day of the surgery wear loose clothes. Do not drink or eat anything for eight hours before the scheduled time. You will have intravenous fluids and anesthetic given.
After the Cornea Transplant procedure
You will be given certain important instructions as to how you should sleep, based on the exact procedure. These need to be adhered to for successful outcome.
DALK or Deep Anterior Lamellar Keratoplasty
What is DALK?
Deep Anterior Lamellar Keratoplasty. As the name suggests it is a type of keratoplasty or corneal transplantation. There have been traditionally two types of replacement of cornea with a cadaver cornea. Full thickness graft referred to as Penetrating Keratoplasty or PK. The other type less commonly used was Lamellar keratoplasty or LK, This is a partial thickness cornea graft. Learn about the Structure of Cornea.
DALK is hybrid between LK and PK. It goes deep where no LK has ever been before (language sounds like Star Trek, huh). It just stops short of the Descemets’ and endothelial layer.
Indications for the DALK procedure
DALK is indicated when the inner layers of the cornea is healthy but the superior layers have a pathology.
Keratoconus Specialist Near Me – In Keratoconus eye disorder the endothelium works but the collagen layer is weak. Keratoconus eye disease is present in younger people. DALK is a good choice in them. If the cornea has ruptured like in Hydrops than DALK may not be possible.
Corneal Dystrophies and superficial scars not treatable with PTK are good candidates for DALK. Scars may varied etiology like post PRK scars, post traumatic or post infective. In cases of herpetic scars it is recommended to wait six months after the active infection has subsided.
Steps in DALK Surgery
- Preparation of patients Cornea: The thickness of the host cornea is measured. Three fourths of this value is calculated. A cornea trephine is set to this thickness.
- A needle is introduced through the trephined edge till it reaches the descemets membrane. An air bubble is introduced till it spreads uniformly across the cornea.
- Lamellar dissection is done with a crescent knife to remove the trephine superficial cornea.
- An air bubble is introduced into the anterior chamber. The constant presence indicates the endothelium has not been perforated.
- The needle is reintroduced into the remaining cornea over the descemets membrane. A knife slits the remaining stroma of the cornea. This is than excised with corneal scissors.
- The donor cornea graft devoid of the inner layer is placed on the bare descemets membrane and sutured with interrupted and/or continuous stitches.
Advantage of DALK Transplant
- Safer during surgical procedure as the eye is closed system. Therefore iris and other content of the eye cannot come out.
- The endothelium of the patient is preserved. The chances of endothelium rejection are avoided.
- Even after DALK procedure eye is more resistant to trauma.
- Induced astigmatism is less.
Disadvantage of DALK
- It is technically more difficult to perform
- It may be necessary to convert it to PK on the operating table.
- The host donor junction can become hazy affecting the best corrected vision.
What exactly is DSEK or Descemet’s Stripping Endothelial Keratoplasty?
Some diseases of the cornea, however, just affect the inner lining of the cornea. A new version of corneal transplant, understood as a Descemet’s Removing Endothelial Keratoplasty (DSEK), has been introduced as a new medical method that utilizes just an extremely slim section of the cornea for transplant. DSEK is a partial corneal transplant technique where the harmful, diseased, posterior part of a person’s cornea is removed and replaced with a healthy and balanced thin corneal graft taken from a cadaver. Unlike the Penetrating Keratoplasty (PK), the DSEK treatment uses only a partial thickness graft. Therefore it requires a much smaller surgical cut and also requires no corneal sutures. This generally results in extra quick aesthetic rehab for the patient as well as reduces the risk of harmful problems that accompany the PK surgery.
Indications for DSEK or Descemets Stripping Endothelial Keratoplasty
When the corneal endothelium is stressed out, the endothelial cells come to be larger and also a lot more thin. As endothelial cell numbers fall in between 500 to 1000 cells/mm, the pump device can no longer preserve a clear cornea. This may occur after prolonged complicated cataract surgery. This entity is termed as Pseudophakic Bullous Keratopathy.
When it comes to Fuchs’ dystrophy the endothelial cells additionally start producing product that makes Descemet’s layer thicker and opaque. Vision at some point deteriorates to a point where these people feel like they are looking through wax paper. Such clients are ready prospects for the DSEK treatment.
Advantages of DSEK or Descemet’s Stripping Endothelial Keratoplasty
There are a lot of major benefits of the DSEK operation in comparison to the normal corneal transplant operation.
- In PK there is a time when the eye is completely open. If the patient were to strain or cough the interior structure of the eye can prolapse forward. In hypertensive patients there is even the chance the retina may come out. This is called expulsive hemorrhage. In DSEK only a small wound similar to that used in cataract eye surgery is made.
- There are many stitches used in PK or penetrating graft. DSEK or Descemets Stripping Endothelial Keratoplasty is either stich less or only one or two sutures may be required
- The chances of rejection are much less in DSEK
- The induced Astigmatism in PK is high compared to the almost negligible amount in DSEK
- Integrity of the eye is better in DSEK than in PK
- Returning to an active lifestyle and resumption of uninterrupted work is faster with DSEK.
The healing with PK can be fairly long, up to twelve months. It is likewise not unusual to have significant irregular curvature of the cornea as a result of the stitches. In many cases a prescription lens is required to achieve the best vision. Finally, a full thickness corneal transplant could have continued weakness even years later on such that even a minor trauma could disjoint the graft from its setting. Cornea specialists have performed DSEK surgery for the past ten years with amazing success. Future endothelial transplant research will center on making the procedure more reliable and not as surgeon-dependent.
Steps of Descemet’s Stripping Endothelial Keratoplasty
The transplant tissue can be made manually by the corneal surgeons in the operating suite. This is done using a special punch and fine dissection. There is a chance of damaging the graft as it is a very delicate procedure. The trend has been to order premade graft from the eyebank. Technicians there do a large number of graft harvesting so they become adept at the procedure. In addition if the graft is damaged they can utilize another donated cornea to yield the graft.
In the event the patient elects to proceed with the surgery, the physician is going to have the patient sign an educated consent form. You’re going to be awake during the process and the majority of people don’t report any discomfort. Dr. K routinely performs this treatment just utilizing eye drops to numb the eye. Some patients could be given local or general anesthesia, especially if their general medical condition is in question.
The DSEK procedure takes approximately 45 minutes to 1 hour. After the eye is prepped and draped in sterile fashion an eye retainer is inserted to keep the eyelids open. The Cornea specialist removes the unhealthy internal cell layer of the cornea. The surgeon implants healthy and balanced benefactor tissue through a tiny cut. Dr.Khanna after that utilizes an air bubble to unfold and place the donor tissue against the patient’s cornea. The small incision is either self-sealing or may be closed with a stitch or two.
Most patients have minimum pain after surgery. Patient is asked to lay flat in the recovery room for about 45 minutes to an hour and is seen again before being discharged home. For the initial 24 hours after surgery patients are requested to lie on their back with their face pointed directly at the ceiling for as much time since they can tolerate. They start to see once the bubble dissolves over the subsequent 2-3 days. They can return to normal activities a week or two following surgery.
Alternatives to DSEK or Descemets Stripping Endothelial Keratoplasty
Since damaged or scarred corneal tissue doesn’t allow light to effectively pass in the eye and get to the retina, bad vision and even blindness may come from a damaged cornea. Patients with a stromal scar as opposed to endothelial dysfunction will require a penetrating keratoplasty rather than a DSEK or Descemets Stripping Endothelial Keratoplasty.
Full Thickness Penetrating Keratoplasty and Lamellar Thickness Keratoplasty have preceded DSEK. Another newer procedure where only Descemet’s is removed is called DWEK. It has only limited indication in certain Fuchs patients. ROCK inhibitors have to be used.
More popular and a finer procedure is DMEK. Here as shown in the picture an even thinner graft is used. The graft here is one tenth the thickness of DSEK.
DISADVANTAGES OF DSEK TECHNIQUE
A difficulty that could occur from the DSEK procedure that is not associated with a conventional transplant is a graft dislocation, where the round disc slips from its desired placement. In this circumstance the donor disc needs to be repositioned in the operating area. If the air bubble escapes the graft may get dislodged requiring another air bubble. The interface between the host and donor is not completely smooth. This may limit vision in few individuals. DSEK also adds more tissue than it removes. It may result in a hyperopic shift.
Here is a DSEK eye surgery video.
When seeking a Los Angeles DSEK or Descemets Stripping Endothelial Keratoplasty surgeon it’s important to select someone with superior knowledge in matters linked to the cornea. Your cornea specialist will have the ability to decide on whether a DSEK partial cornea transplant is the ideal procedure for you.
DMEK or Descemet’s Membrane Endothelial Keratoplasty
DMEK or Descemet’s Membrane Endothelial Keratoplasty is the latest advancement in corneal transplant surgery. It is a newer variant of DSEK corneal surgery. It involves transplanting only the inner 15 microns of the cornea.
Indications for DMEK
It is indicated in Fuchs dystrophy, Pseudophakic Bullous Keratopathy and other corneal diseases limited to the innermost lining of the cornea. A prerequisite is that the rest of the cornea should be healthy. If there is opacity in the center of the cornea than a full thickness graft may be more appropriate. Handling this ultra thin graft requires a high level of dexterity. This behooves a clear view beneath the cornea. The upper layer of the cornea called the epithelium can be removed to improve clarity.
THE DMEK PROCEDURE
The procedure consists of three parts. Harvesting the graft from the donor cornea is the first step. Next the recipient cornea is prepared to receive the graft. Finally the endothelial graft is introduced into the patients eye and made to stick to the cornea.
STEP 1 OF DMEK
The donor cornea is put endothelial side up in a punch like a Moria disposable punch. A dull instrument is used to separate the descemets from the schwalbes’ line. When approximately 60 percent has been cleaved the corneal button is centered over four holes. It is then stained with trypan blue. It is than punched with a 7.5 mm to 8 mm trephine. The descemets is separated from the rest of the cornea. It is soaked in trypan blue and covered. Attention is than directed to the patient.
Nowadays surgeons are preferring to obtain a precut preloaded prepared graft. This graft already has a mark to determine its orientation.
STEP 2 OF DMEK PROCEDURE
The patients eye is prepped and draped. Some surgeons proceed with topical anesthetic drops. Others prefer to perform a retrobulbar block to prevent eye movements. A speculum is inserted. The center of the cornea is identified. A ring of 8mm is placed over it. The indentation are marked with a marking pen. Two 1 mm paracentesis incisions are made. Viscoelastic is injected in the eye.The main temporal wound is 3 to 5 mm . A reverse sinksy instrument scores the descemets’ and endothelium along the preinked corneal marks. This tissue is than stripped off. A forceps grabs it. It is than placed over the cornea to confirm it is uniform. Also the inner cornea is inspected to detect if there are any strips of the tissue left behind. An opening is made in the iris at 6 or 9 o’clock. If all is fine the viscoelastic is removed. Any residual viscoelastic is an enemy to the donor graft says Dr.Khanna
STEP 3 OF DMEK
Now is the most challenging part. The graft is loaded into a specially designed bulbous glass device attached to a syringe. Hence the graft gets curled with the endothelial side up. This device is introduced into the temporal wound. With gentle pushes the graft is pushed into the anterior chamber of the eye. Then the dance begins as we want the graft to unfold. The cornea is gently tapped and rolling motions executed. An air bubble is introduced under the flap once it opens. The remarked S or F is identified to confirm it is right side up. Air is introduced to raise the pressure of the eye for next 10 minutes. Then some of the air is released. A subconjunctival injection of steroid and antibiotics is given.
Patient is transferred but made to lie flat on their back for the next hour. They are also instructed to do the same at home.
DWEK or DSO is a type of Corneal graft.
Well in a recent post we talked about DSEK and DMEK. These are alternatives to full thickness penetrating corneal grafts. They also may be called sutureless corneal graft.
Now one of the surgeons whose DMEK graft fell off discovered the cornea still healed. The realization dawned that removing just the diseased endothelium may all that is required in certain patients. This procedure is called DWEK or DSO. DWEK stands for Descemets stripping without Endothelial Keratoplasty. A more apt name may be DSO Descemets stripping only.
This is shown to work in few selected individual. The best candidate might be an older person with just central dense Fuchs guttate. Central 4 mm of endothelium is removed. The adjoining healthy cells migrate and take over the function of the unhealthy cells. The cornea clears and vision improves. This process can take 3-4 months.
DMEK clears up the cornea faster and is preferred in younger individuals. DSEK is the original procedure which involved removing of the unfit inner corneal cells. Actually all these surgical interventions are a continuum of inner corneal transplants. The difference being how much of the diseased cornea is removed. And whether a transplant is performed. If performed than the thickness may vary.