Welcome to Khanna Vision Institute: Your Los Angeles Ophthalmologist
Transform Your Vision With the Best Laser Eye Surgery in Los Angeles
Welcome to the Future of Vision. Khanna Vision Institute offers state-of-the-art, safe, and painless laser eye surgery in Los Angeles. Dr. Rajesh Khanna, Medical Director, is one of the most experienced ophthalmologists in Beverly Hills and the surrounding area. Our comfortable, welcoming offices serve patients of all ages
Do you dream of clear vision without the need for glasses or contact lenses?
Under 45 Years
The best options for young adults
Above 45 Years
When reading near is an issue.
All Ages
Young & Mature – KVI is here

Procedures We Offer
- Painless Lasik
- Superlasik
- EVO ICL
- SuperLasik
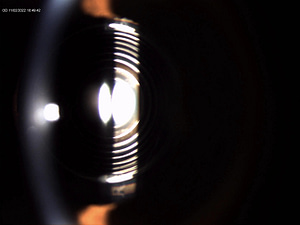
- PIE Procedure (Presbyopic Implant in Eye)
- Laser Cataract Surgery
- Cornea Cross Linking For Keratoconus
- Cosmetic Pterygium Treatments
We have offices in Beverly Hills, Westlake Village, Inglewood, Sherman Oaks, Moorpark, and Oxnard. Clear vision begins when you schedule a free in-person or remote consultation.
Get in touch and discover the best vision procedure to suit your needs. Be sure to ask how our painless lasik can enhance your life.
Awards and Recognition
Good patient care and great surgical outcomes get recognized and appreciated.

Super Doctors So Cal
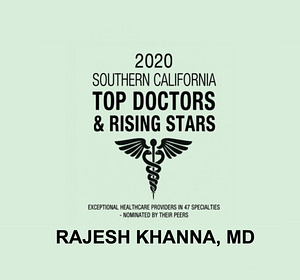
Top So Cal Doctors

Newsweek showcase
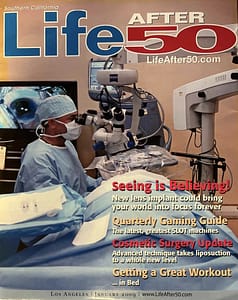
Life After 50
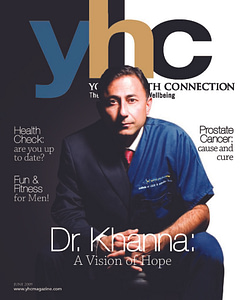
YHC Cover

Daily News Readers
Your Vision Goals Are Our First Priority

Smiling Surgeon
Khanna Vision Instittues strives to deliver the best. Our goal is to see a smile on your face during every appointment. That makes the staff and Dr. Khanna Happy too. Learn what makes Dr. Khanna the best ophthalmologist in Los Angeles.

Smiling Patients
We understand your fears, anxieties, and expectations. Safety comes first. We deploy the latest technolgy to choose what’s best for you. Discover why patients consistently choose Khanna Vision Institute for laser eye surgery in Los Angeles.
Vision Correction Procedures
At Khanna Vision Institute we know each eye and each person is unique. We offer various refractive surgical procedures, from Lasik, to ICL, to SMILE, so the results always meet patient expectations. Our team will recommend the safest and most effective procedure for your unique eyes and goals. Learn more about the laser eye procedures we offer at Khanna Vision Institute below.

Remote Eye Exams
Your busy schedule may not allow you to come to our main office. We have deployed state of the art technology to allow to do a detailed remote exam. Visit our satellite offices to experience top-quality care with unmatched convenience.